Introduction
ITP is characterized by low platelet count due to immune mediated destruction and bleeding tendency. However, during last few decades thromboembolic events have been reported in patients with ITP.
This review is done to study the reported cases of thromboembolic phenomenon in patient with ITP in an attempt to assess the patient characteristics and to understand the underlying mechanism.
Methods
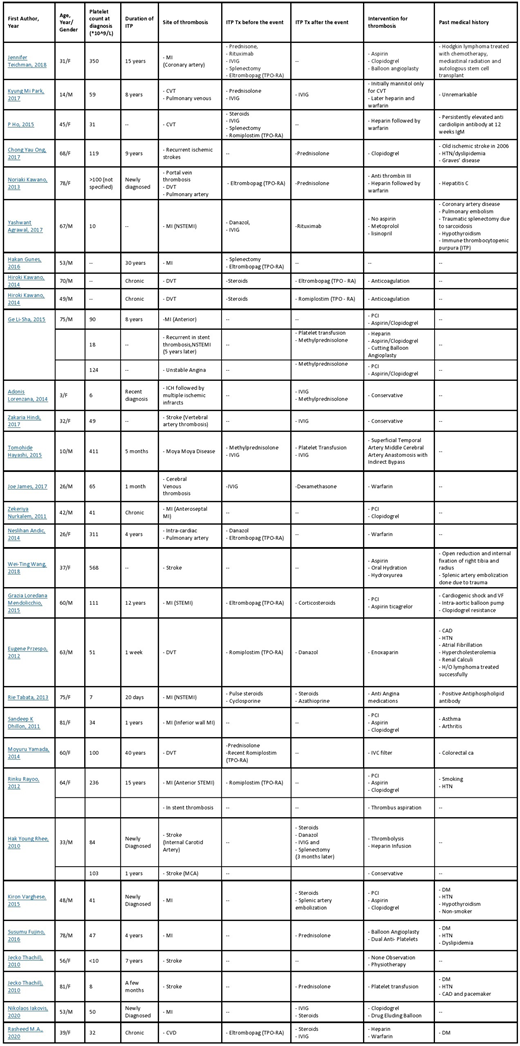
We searched google Scholar, PubMed about cases with ITP and thrombosis the summary is presented in the following table (Table 1).
Results
Around 30 reported cases of ITP with thrombotic events were identified and a total of 36 events were recognized in last 10 years.
The ages ranged from 3 years to 81 years with a mean of 51 years.
Most of the patients were young and middle aged (18-65 years of age), meanwhile around 9 patients were elderly (age > 65 years). Only 3 cases were observed in pediatric age.
Almost equal incidence in both genders was recognized.
Half of the patient had chronic ITP while in the rest it was diagnosed less than a year.
20 out of 36 (55.6%) events happened at platelet count less than 100*10^9. While 16 events were reported with platelet count higher than this or unknown.
Majority of the patients (around 64%) developed arterial events while fewer developed venous thrombosis.
For treatment, most of the patients (44%) were not receiving any particular treatment for ITP at the time of thrombotic event. While 6 events (17%) happened while being treated with IVIG and 10 events (28%') happened while on TPO-RA. Only 3 patients were treated with corticosteroids prior to the event.
In patients treated with TPO-RAs arterial and venous events were almost similar (57% vs 43% respectively) while majority of the events happened at lower than normal platelet count (7/10 events).
Almost half of the patients had one or more underlying risk factor predisposing to atherosclerosis and thrombosis.
Most of the patients were treated appropriately for the events with either antiplatelet agents or anticoagulation while simultaneously treatment for ITP was given. Corticosteroids were most frequently used for ITP during the episode followed by IVIG (52% and 28% of total treated patients respectively). Only 1 patient was treated with TPO-RA after the event for low platelet counts while others received other treatments (Rituximab, Danazol and splenectomy).
Discussion
Thrombosis is a complex process involving arteries and veins. Accelerated atherosclerosis and plaque rupture is the underlying event for arterial thrombosis. While in venous thrombosis immobility and procoagulant states are the main factors.
Immune thrombocytopenia is characterized by immune mediated destruction and impaired production of platelets predisposing to bleeding mostly. However, it is a unique pathological process that is linked to both bleeding and thrombosis.
Multiple factors predispose patients to thrombosis in ITP. The patients with chronic and active disease are particularly at risk of paradoxical thrombosis due to accelerated atherosclerosis as in other autoimmune conditions, predisposing to arterial thrombotic events.
Active disease is also characterized by increased turnover of platelets in bone marrow and higher levels of circulating platelets microparticles (PMPs) which promote thrombin formation and promote venous thrombosis.
The patients treated with IVIG and TPO-RA are at higher risk as compared to other forms of treatment.
IVIG is used in acute states as it prevents the destruction of platelets but simultaneously promotes thrombosis by increasing blood viscosity and thrombin production.
TPO-RAs are agents which mimic the action of thrombopoietin on megakaryocytes promoting their growth and differentiation and increasing platelet production. Increasing platelet count above the normal target might contribute to thrombosis however megakaryocyte activation itself leads to increased risk of thrombosis, despite low platelet count.
In patients with ITP and thrombotic events, judicious use of antiplatelet therapy and anticoagulation is indicated along with simultaneous therapy directed at improving platelet count.
Conclusion
Patient with active ITP are predisposed to thrombosis in addition to bleeding. A treating physician needs to be vigilant to diagnose early the events and then to institute proper use of antiplatelets and anticoagulation along with therapy directed at ITP.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal